Here is some great info on B12.
The human body requires thirteen different vitamins to maintain health and sustain life. These molecules participate in many thousands of chemical reactions which play significant roles in building tissue and maintaining the functional vitality of organs. Vitamins participate in processes that ultimately provide the body with useable energy, eliminate toxins, protect against infection, repair cellular damage and invoke inter-cellular communication. The human body unable to synthesize vitamins must for the most part acquire them from food. Some vitamins are fat-soluble and once ingested are readily stored while others are water-soluble and incapable of accumulation. Failure to take in, absorb and make use of sufficient amounts of each vitamin brings about a deficiency which in turn leads to disease and eventually the possibility of death…
One of the thirteen vitamins is water-soluble vitamin B12 known as cobalamin. Cobalamin is an unusual molecule and unlike any of the other twelve vitamins contains a trace element – cobalt. It is “nature’s most complex non-polymer molecule and the most complex of the vitamins and enzymatic co-factors.” 1 Although cobalamin is present in diets containing meats and dairy products and its daily requirement in man is miniscule (4 micrograms) forty percent (40%) of the U.S. population, young and old have low to deficient levels.” 2
Researchers at Tufts University analyzing data from the very comprehensive Framingham Offspring Study 2 found no association between plasma B12 and meat, poultry and fish intake, even though those foods supply the bulk of B12 in the American diet. In the words of one researcher “It’s not because people aren’t eating enough meat. The vitamin isn’t getting absorbed”. 2
Very few doctors seem to be aware of the diversity of problems that can come about from inadequate levels of Vitamin B12. Part of this failure resides in the belief that B12 deficiency is simply a blood disorder and as a result B12 is examined only within the context of anemia. As a consequence inadequate levels of vitamin B12 can develop and damage brain, spinal cord, peripheral nerves and optic nerves well before blood abnormalities manifest themselves.
This failure of misdiagnosis is further explained by the regularity of which symptoms of deficiency mimic those of dementia, psychosis, depression, vertigo, tremor, neuropathy, recurrent miscarriages, infertility, vision loss, fatigue, dizziness, autistic-like disorders, etc.
Perhaps the primary reason doctors roll their eyes at the mention of vitamin B12 is they are programmed to react that way. Vitamin B12 many decades ago was over prescribed for “whatever ails you”. Country doctors increased revenue by over-selling it to patients. Over time a taint developed which stuck to vitamin B12. No legitimate well-educated doctor wants to be involved in the selling of tonics and today that stigma is associated with Vitamin B12.
What has slowly been scientifically emerging though and is not widely disseminated in the medical community is that cobalamin is involved integrally in neurologic, hematologic, immunologic, metabolic, vascular and reproductive functions such as:
- cellular division and transmission of the genetic code to all newly formed cells through production of both DNA and RNA (most evident in bone marrow and myeloid cells);
- enzymatic reactions (primarily methyl group transfer and transfer of a hydrogen atom from one carbon to an adjacent carbon atom);
- synthesis of nucleic acids, the transmethylation of amino acids and the metabolism of carbohydrates and fatty acids;
- maintenance of a healthy nervous system (by maintaining the myelin surrounding nerves);
- proper functioning of folic acid by assisting in converting the amino acid homosysteine into methionine. If B12 is not present folic acid becomes trapped, which leads to dangerous elevations in toxic homocysteine.
It is the failure of cobalamin to carry out its role in these vital functions that leads to medical symptoms often mistaken for more untreatable diseases such as multiple sclerosis. If left unremedied vitamin B12 deficiency can eventually reduce the body to a state of permanent disability.
The complexity of the absorption and transport process lends itself to the potential for failed cobalamin uptake in everyone. The following people however seem to be at greatest risk of deficiency:
- Users of:
- metformin (glucophage) and similar diabetic drugs;
- stomach acid suppressors (proton-pump inhibitors, H2-blockers, antacids);
- alcohol;
- certain drugs(Questran, Colchicine, Neomycin, Dilantin, potassium chloride, para-aminosalicylates)
- People who:
- are Vegetarians;
- have had any gastric or intestinal surgery;
- have undergone surgeries or dental procedures involving nitrous oxide;
- are over the age of sixty;
- have a family history of pernicious anemia;
- have intestinal diseases (Crohn’s, irritable bowel syndrome, celiac, malabsorption of nutrients, etc.);
- have autoimmune disorders especially thyroid and type 1 diabetes;
- have undergone certain radiologic cancer treatments;
- Women with histories of infertility or miscarriages; and
- Infants born to and breast fed by women who are deficient.
Yet everyone, irregardless of age or apparent health possesses the potential to become deficient. Uptake of vitamin B12 seems to be bit by bit, while certain events (most inflammations for instance) can lead to a draining of vitamin B12 which is not always replenished by dietary uptake.
This is such a crucial point that it is worth reemphasizing. One of the most comprehensive studies ever undertaken was the Framingham Offspring Study which examined about 3,000 men and women who were the children of people in an original study (Framingham study) that focused on cardiovascular disease risk factors. Researchers analyzed that data and found that thirty-nine percent (39%) of the participants had plasma B12 levels in the “low normal” range – below 258 picomoles per liter. As the study leader Katherine L. Tucker pointed out, “this is above the currently accepted deficiency level of 148 pmol/L however some people exhibit neurological symptoms at the upper level of the deficiency range”. 2 Katherine L. Tucker is very well respected in her field. She is a nutritional epidemiologist at the Jean Mayer USDA Human Nutrition Research center on Aging at Tufts University in Boston. When she states “I think there’s a lot of undetected vitamin B12 deficiency out there” 2 it is significant. The results of the study found that the youngest group, the 26 to 49 year olds had about the same vitamin B12 status as the oldest group, 65 years and up 2.
So pay attention, because this article speaks to either you or someone you care about.
References:
1 – Wheatley, Carmen, A scarlet pimpernel for the resolution of inflammation? The role of supra-therapeutic doses of cobalamin, in the treatment of systemic inflammatory response syndrome (SIRS), sepsis, severe sepsis, and septic or traumatic shock, Medical Hypotheses (2006) 67, 124–142
2 – Tufts University Researchers analyzing data from the Framingham Offspring Study, discussed in B12 deficiency may be more widespread than thought, Judy McBride, Agricultural Research Service, U.S. Department of Agriculture, August 2, 2000 B12 Deficiency May Be More Widespread Than Thought / August 2, 2000 / News from the USDA Agricultural Research Service
3 – In general: The writings, reports and internet postings of Sally M. Pacholok, R.N. (a studied expert on the topic of Vitamin B12 Misdiagnoses)
4 – In general: Drawn from my reading of the articles cited herein.
Hunger
It was established more than half a century ago that Vitamin B12 intake increases feelings of hunger in both humans and animals which leads to increased food intake and the potential for subsequent growth.
In a study carried out by
Wetzel, vitamin B12 was orally administered to children who were in various states of recovery from growth failure or who exhibited slow progress. The study found that the “clinical changes after B12 administration were those of increased physical vigor, alertness, better general behavior, but above all, a definite increase in appetite, manifested by demands for second helpings, as contrasted with comparatively indolent food habits before” 1. Increases in the appetites of children were found in several other studies during this time period specifically attributable to vitamin B12 8,9,11.
In pigs, the addition of vitamin B12 was found to increase daily feeding per from 2.57 pounds of food and an average weight gain of .87 pounds per day to that of 3.21 lbs of feed consumption and a 1.2 lb per day body weight gain. These results led the authors to conclude that “the significantly greater gains made by pigs in lot 2 were [likely] due to the addition of vitamin B12 concentrate” 2.
In a study carried out in mice, the authors noted that “the difference in growth rate resulting from the administration of increasing amounts of vitamin B12 is very striking… Increasing the daily administration of vitamin B12 from 0.001 to 0.01 grams resulted in a growth increment during the 15-day test period of approximately 4 grams in the case of the thyroid-fed mice but of only 1 gram in the low fat group. This increase in growth rate was attributed to B12′s effect at increasing food intake”. 3
Although the ratio is not specifically relevant to humans, it is interesting to note that in pigs it was found that vitamin B12 administered orally required dosages 5 to 10 times higher than administration by injection to achieve the same effect4.
In another study involving rats receiving vitamin B12 and eating ad libitum, it was found that they grew more rapidly, ate more of the diet and retained more nitrogen than their controls. The conclusion of the study was that Vitamin B12 was associated with increased growth, food intake and nitrogen balance 5.
In an early study involving humans and the entire vitamin B complex, a supplementary ingestion of approximately 150 units of vitamin B (representing an increase of about 50% in the daily vitamin B intake) produced increases of from 17 to 25% in the grams of food consumed per child per day. The caloric ingestion during these periods of increased food consumption correlated to a slight degree with increased weight gains11.
So how does Vitamin B12 Increase Hunger?
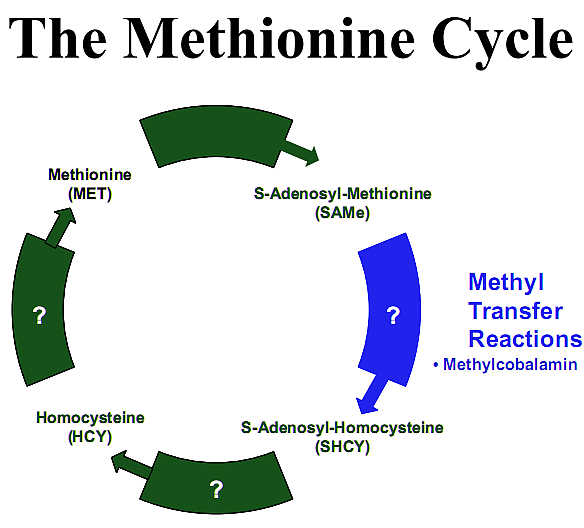
There are probably multiple reasons. However one reason may be its participatory role in the conversion of Histamine to N-methylhistamine. As a methyl donor (meaning that chemically it gives up its methyl group), methylcobalamin reduces homocysteine to methionine (because homocysteine + methyl group = methionine) via a process known as “The Methionine Cycle”12.
Methionine is converted back into S-Adenosyl-Methionine (SAMe) by giving up its methyl group to a number of different compounds. In this way many types of methylated compounds are produced13.
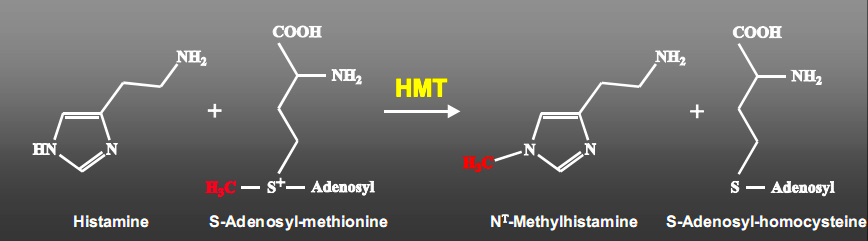
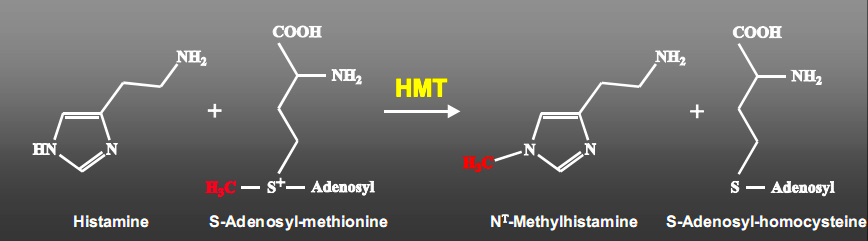
One of those compounds is N-methylhistamine. The enzyme “Histamine N-methyltransferase” (HMT) catalyzes the transfer of a methyl group from S-Adenosyl-Methionine (SAMe) to the secondary amino group of the imidazole ring of Histamine forming N-methylhistamine14.
So to reiterate and pick up an earlier step, cobalamin assumes two principal forms one of which is methylcobalamin. When hydroxocobalamin is transported into cells via the transcobalamin II transport protein (TCII), this transporter is degraded and hydroxocobalamin converted into 5-deoxyadenosylcobalamin which acts in the mitochondria and methylcobalamin which acts in the cellular cytoplasm. It is there that methylcobalamin is used in the Methionine Cycle to recycle Homocysteine back to Methionine. In this reaction B12 is the cofactor for the enzyme Methionine Synthase (these are the two initiators of this process). Methionine is an essential amino acid that is used to make SAMe. SAMe is the body’s primary methyl donor for methylation reactions. One of those reactions indirectly converts Histamine to N-methylhistamine.
How does converting Histadine to N-methylhistamine increase hunger?
Alterations in brain histidine (and histamine) concentration are associated with changes in food intake. There is an inverse relationship between brain histidine (and histamine) and food intake such that elevated levels reduce hunger and reduced levels increase hunger15.
In addition the central histamine receptors (H1, H2 and H3) are involved in the regulatory process. Antagonizing histamine H1 receptors stimulate appetite and weight gain16-20.
On the other hand, it has been found that cerebroventricular infusion of an H3 receptor antagonist (thereby increasing synthesis and release of brain histamine) reduces hunger and depresses feeding in rats21.
However those compounds that are H3 receptor agonists (they decrease synthesis and release of brain histamine) increase hunger and feeding. N-Methylhistamine is an agonist at H3 receptors22,23.
So it would be expected that decreasing the amount of appetite suppressant (histamine) by converting it to an appetite stimulant N-Methylhistamine would have an overall effect of increasing appetite. This increased hunger effect was discovered more then half a century ago.
References:
1 – Wetzel, Norman C. et al., Growth Failure in School Children as Associated with Vitamin B12 Deficiency—Response to Oral Therapy, Science 16 December 1949 110: 651-653
2 – Lueck, B. W. 1949, The Effect Of Vitamin B12 Concentrate On The Growth Of Weanling Pigs Fed Corn-Soybean Diets AScience, 110: 139
3 – Bosshardt, D. K., W. J. Paul Ande. H. Barnes 1950, The Influence Of Diet Composition On Vitamin B12 Activity In Mice, J. Nutrition , 40: 595
4 – Anderson,G. C., Anda. G. Hooan 1950, Requirement Of The Pig For Vitamin B12, J. Nutrition, 40: 243
5 – Ralli, E., et al., The Effects In Rats Of Vitamin B12, With And Without Ethyl Alcohol, On Nitrogen Balance, Serum Albumin, Liver Nitrogen And Fat, J. Nutr., Jan 1959; 67: 41 – 57
6 – Ershoff, B. H. 1947, Comparative Effects Of Liver And Yeast on Growth And Length Of Survival Of The Immature Thyroid-Fed Rat, Arch. Biochem., 15: 365
7 – Rupp, J., K. E. Paschkisanda. Cantarow 1951, Influence Of Vitamin B12 And Liver Extract On Nitrogen Balance Of Normal And Hyperthyroid Rats, Proc. Soc. Exp. Biol. Med., 76: 432
8 – Wilde, E., The treatment of growth failure in Aleut school children, J. Pediat., 40: 565, 1950
9 – Larcomb, J. W., Perry, C. S., and Peterman, R. A., Dietary supplementation of vitamin B12 in prepuberty school-age children, J. Pediat., 45:70, 1954
10 – COMMITTEE ON NUTRITION: Appraisal of the Use of Vitamins B1 and B12 as Supplements Promoted for the Stimulation of Growth and Appetite in Children, Pediatrics, May 1958; 21: 860 – 864
11 – Schlutz F. W., et al., The Effect Of Varied Vitamin B Ingestion Upon The Appetite Of Children, The Journal of Nutrition, Vol. 15, No. 5 May, 1938
12 – Wheatley, Carmen, A scarlet pimpernel for the resolution of inflammation? The role of supra-therapeutic doses of cobalamin, in the treatment of systemic inflammatory response syndrome (SIRS), sepsis, severe sepsis, and septic or traumatic shock, Medical Hypotheses (2006) 67, 124–142
13 – Springer Handbook of Enzymes Volume 28, Springer Berlin Heidelberg 2006, pages 43-50
14 – Schwelberger HG, Histamine N-methyltransferase (HNMT) enzyme and gene. In Falus A (ed). Histamine: Biology and Medical Aspects, SpringMed Publishing, Budapest, 2004: 53-59
15 – Mercer, L. P., Manipulation of Central Nervous System Histamine or Histaminergic Receptors (H1) Affects Food Intake in Rats, J. Nutr. 124: 1029-1036, 1994
16 – Kalucy, R. S. (1980), Drug-induced weight gain, Drugs 19: 268-278
17 – Kanba, S. & Richelson, E. (1991), Interactions with psychotropic drugs. In: Histaminergic Neurons: Morphology and Function (Watanabe, T. & Wada, H., eds.), pp. 271-282, CRC Press, Boca Raton, FL.
18 – Lavenstein, A. F., Dacaney, E. P., Lasagna, L. &. Van Metre, T. E. (1962), Effect of cyproheptadine on asthmatic children, JAMA 180: 912-916
19 – Noble, R. E. (1969), Effect of cyproheptadine on appetite and weight gain in adults, JAMA 209: 2054-2055
20 – Silverstone, T. & Schuyler, D. (1975), The effect of cyproheptadine on hunger, caloric intake and body weight in man, Psychopharacologia 40: 335-340
21 – Machidori, H., Sakata, T., Yoshimatsu, H., Ookuma, K., Fujimoto, K., Kurokawa, M., Yamatodani, A. & Wada, H. (1992), Zucker obese rats: defect in brain histamine control of feeding, Brain Res. 590: 180
22 – Beales, I. and Calam, J., The histamine H3 receptor agonist N-methylhistamine produced by Helicobacter pylori does not alter somatostatin release from cultured rabbit fundic D-cells, Gut. 1998 August; 43(2): 176–181
23 – Courillon Mallet A, Launay JM, Roucayrol AM, et al., Heli-cobacter pylori infection: physiopathologic implication of N alpha-methyl histamine, Gastroenterology 1995;108:959–66
Anecdotal reports on the effectiveness of long-term supra-physiological administration of Vitamin B12
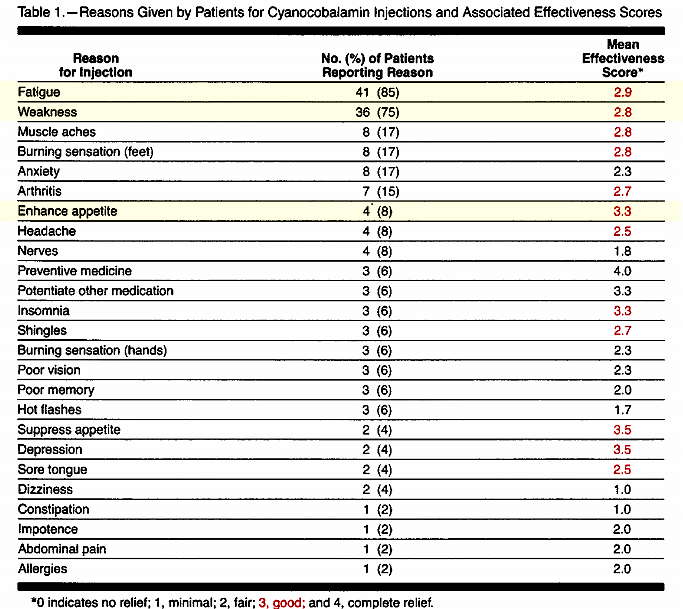
In 1987 a small town medical clinic witnessed the retirement of it’s general practitioner; a doctor who had practiced by himself in that facility for more then forty years. The clinic was taken over by a new doctor and the case files reviewed. It was discovered that 120 patients had been receiving regular cyanocobalamin (vitamin B12) injections for an average of ten years. Only 4 of those patients however met the current doctor’s criteria for continuing administration. A number of the patients were interviewed to find out their reasons for accepting Vitamin B12 administrations and on a scale of 0 to 4 rated the effectiveness of treatment. The scale was such that 0 represents “no relief”, 1 represents “minimal relief”, 2 represents “fair relief”, 3 represents “good relief” and 4 represents “complete relief”. 1
The patients were then presented with discussion concerning the reason that the doctor felt they did not need vitamin B12. The results of this persuasion were reported in a study which appeared in JAMA with the sole focus of demonstrating that patients could be persuaded to give up vitamin B12. They were able to persuade 62% to give up their injections. 1
The choice of words by the authors of that study reveals their bias when they state, “Anecdotal evidence suggests widespread use of cyanocobalamin as a
tonic or as treatment for nonspecific complaints.”
What is more interesting is that 18 patients (38%) who were younger and who reported greater symptom relief refused to give up the Vitamin B12 injections despite the “persuasive evidence” of the new doctor and stated that they would actively seek a physician who would continue to administer cyanocobalamin.1
The most interesting part of the study is the table reproduced below which indicates which ailments the patients had received vitamin B12 for and their perception of effectiveness. Keep in mind that of the 120 patients, 86 were women and 34 were men with a mean age of 71 years. However they had been receiving the administrations for an average of ten years.1
I believe this report is a solid survey of people who are in a position to report the effects of long-term usage. Notice that the largest group of patients received the shots to fight fatigue and weakness. They reported that they had experienced “good relief”.1
It is also noteworthy that in those that used vitamin B12 to increase hunger the effectiveness rating was between good and complete relief.
References:
1 – Lawhorne L MD and Ringdahl, David MD, Cyanocobalamin Injections for Patients Without Documented Deficiency: Reasons for Administration and Patient Responses to Proposed Discontinuation, JAMA 1989;261:1920-1923
Vitamin B12 a Master Molecule
If you are someone who uses vitamin B12 solely to reduce fatigue and increase hunger you may be of the mind that the remainder of this article is not directly applicable to you.
The rest of the article will explore the misdiagnosis of vitamin B12 as a medical failure that may lead to needless suffering in people you care about. Perhaps as a result of what you are about to read you will be in a better position to prompt others around you to demand to be tested properly and to seek accurate diagnosis of their current health problems: Problems that neither they nor their doctors attributed to depletion of this crucial molecule.
In addition the article will touch on vitamin B12′s newly discovered ability to act as an intracellular antioxidant, its role in inflammatory states and the current hypothesis that it is the concentration of vitamin B12 that the body attempts to increase within damaged tissue in disease states. These sorts of things are novel and are directly applicable to everyone irregardless of their current levels.
Deficiency
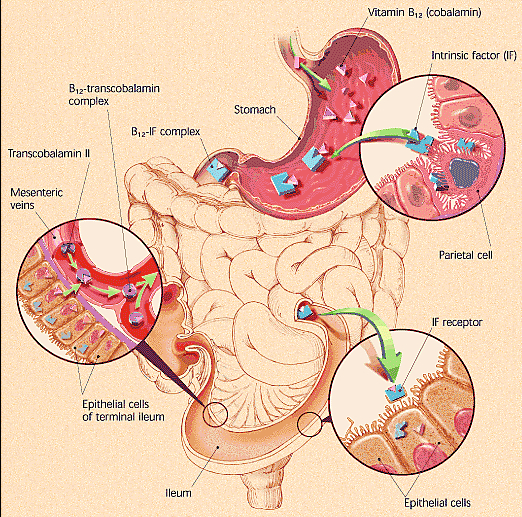
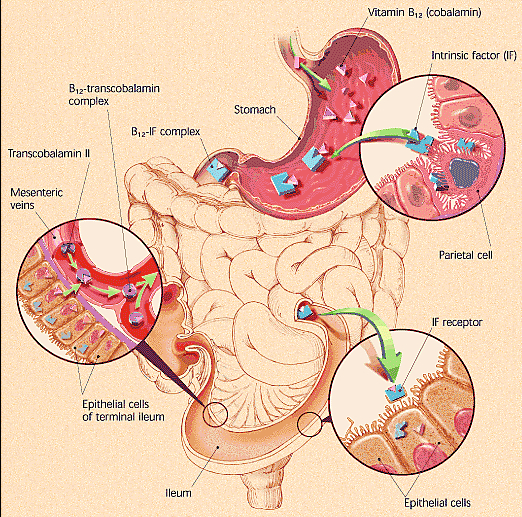
Absorption of vitamin B12 from food is complex. The vitamin B12 in food is bound to animal protein and must be cleaved via the enzyme pepsin. Pepsin can only be produced in adequate amounts if the stomach contains enough hydrochloric acid. Once isolated B12 is carried to the small intestine by proteins called R-binders. In the intestine, intrinsic factor (IF) which is made in the stomach, attaches to B12 with the assistance of enzymes called pancreatic proteases and carries it to the final section of the small intestine, the ileum. The cells that line the ileum contain receptors that grab the B12-IF complex pulling it into the bloodstream.35
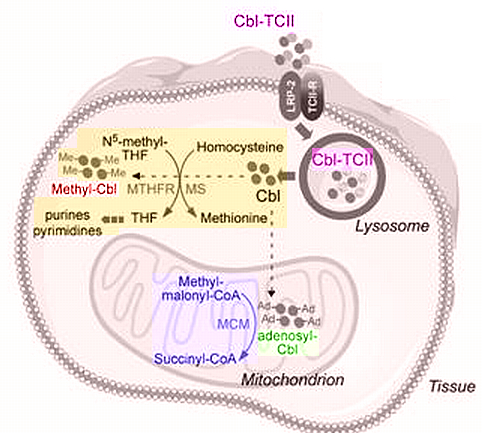
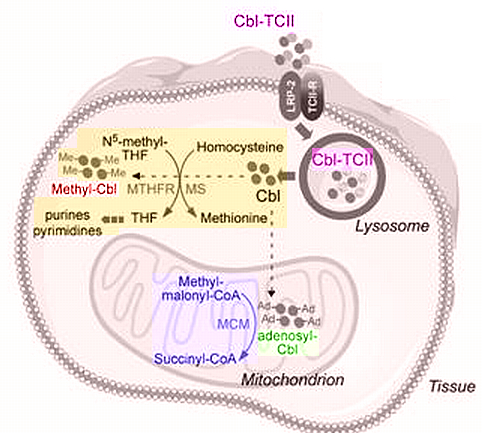
In the bloodstream, another protein, transcobalamin II (TCII) carries vitamin B12 which started as cobalamin but at the stage of entering the blood stream is in the form of Hydroxocobalamin. The carrier protein, Transcobalamin II (TCII) bound to Hydroxocobalamin enters cells in all tissues via the TCII endocytosis ion channel receptor where after TCII degradation it is converted to Methylcobalamin and 5-deoxyadenosylcobalamin and primarily retained intracellularly. A small portion is however exported via the carriers TCII and Transcobalamin III (TCIII). Methylcobalamin acts in the cytoplasm where it is involved in the Methionine Cycle and 5-deoxyadenosylcobalamin in the mitochondria where it is involved in the Krebs cycle (cellular energy).35
This complexity of the vitamin B12 metabolic process greatly exceeds that for any other vitamin and may fail at any one point. The most well known breakdown point, although not the most common is pernicious anemia. This disease occurs when the body fails to produce intrinsic factor (IF) making dietary B12 useless.
Less well-known but more common breakdown points result in lower amounts of vitamin B12 absorption from either food or oral supplementation. Once someone becomes deficient , the few micrograms from standard supplementation will fail to meet the immediate need for thousands of micrograms.
Loss of brain function isn’t always incurable
“Many people do suffer from Alzheimer’s and other dementias but some who are labeled as having dementia are actually suffering from problems that can be corrected”, writes neurologist Sydney Walker III, M.D. Studies suggest that up to 60 percent of patients tentatively labeled as having dementia actually have treatable reversible disorders.1
There is no test that can diagnose Alzheimer’s conclusively in a living patient. The only way to differentiate between Alzheimer’s and other causes of dementia is to rule out all other causes. This is rarely done. In Finland, a study found that only 20 percent of patients with symptoms of dementia were screened for vitamin B12 deficiency.2
Not only is a serum vitamin B12 test too infrequently ordered by physicians it is inadequate. Many seniors with borderline or normal serum B12 levels are severely deficient to the point of developing Alzheimer’s-like dementia. This test gives false positives and negatives and is not sensitive enough. Because of these limitations a Urinary Methylmalonic Acid (MMA)/creatine ratio test should be given. It is an extremely accurate test capable of confirming or ruling out B12 deficiency.3
Dr. Eric Norman the inventor of the test used the MMA test to re-evaluate 299 seniors whose B12 results had tested normal using the standard serum B12 test the year before. The retesting discovered that 2 percent had vitamin B12 deficiency. For thirty million United States elderly, 600,000 new cases per year are going undiagnosed.3
Vitamin B12 deficiency often strikes the nervous system causing damage to the soft fatty material called myelin that surrounds and protects nerve fibers. This damage (akin to a fraying of electrical wires) can cause mysterious and painful neurological problems from numbness, tingling, painful limbs, balance problems, vision loss, incontinence, impotence, memory loss, fuzzy thinking, personality changes, depression and dementia.
This can lead to immune system problems as the body begins to fail to produce sufficient white blood cells. The body becomes more susceptible to infections and viruses. Gastrointestinal problems may occur with the loss of ability to regenerate lining.
Feelings of exhaustion may develop due to anemia when the body is unable to carry sufficient oxygen to cells in the body.
Breakdown in the metabolic pathway (The Methionine Cycle) that detoxifies homocysteine occurs which increases risk of coronary, artery disease, stroke and blood clots.
The lining of the uterus and cervix can become compromised leading to opportune cancers.
The failure to initially diagnose vitamin B12 deficiency and treat it results in a lost opportunity to halt a cascade of problems. Most of these problems will be treated by drugs and therapies none of which attack the root of the problem. With the passage of time eventually remedying the root of the problem with B12 restoration may come too late. The damage that was done will not become undone. There seems to be a critical window of opportunity for treating B12 deficiency and therapy started more than six months after the onset of symptoms may fail to reverse symptoms.
Dr. Mark Goodman reported treating 24 demented patients whose seemingly normal serum B12 levels masked a severe B12 deficiency. When he gave these patients B12 injections every one of them improved dramatically.4
These problems are not confined to the elderly. A twenty-one year old woman who developed bipolar disorder and then full-fledged dementia both due to deficient B12 levels and an accompanying folate deficiency was treated with vitamin B12 and in the words of her doctor experienced a “dramatic resolution” of her symptoms.5
Alzheimer’s
There is some evidence that deficient vitamin B12 levels not only worsen Alzheimer’s symptoms but may possibly play a role in bringing about the disease. The evidence is speculative.
In a study 6 by Robert Clarke levels of B12, folate and homocysteine in 164 of his patients diagnosed with Alzheimer’s were measured and compared to a non-diseased control group. Seventy-six of those patients subsequently died and autopsies confirmed that they did in fact have Alzheimer’s. They found that 6:
- homocysteine levels at the patients’ initial visits were significantly higher in the Alzheimer’s group then the control group;
- B12 and folate levels were significantly lower in the Alzheimer’s group;
- Alzheimer’s patients with high homocysteine levels showed greater evidence of disease progression a trend followed by B12 and folate as well;
- Homocysteine levels in the Alzheimer’s patients didn’t change as the disease progressed indicating that the differences between patients and control group members weren’t caused by the disease itself, but rather predated or coincided with the onset of the disease
He speculated that high levels of toxic homocysteine possibly resulting from B12 deficiency, may cause microinfarcts (tiny areas of blood vessel damage) that then trigger the formation of the plaques and tangles that eventually clutter the brain of a person with Alzheimer’s.6 Robert Clark then concluded “low blood levels of folate and vitamin B12 and elevated total homocysteine levels were associated with Alzheimer’s disease.” 6
In another study demonstrating correlation, researchers found that four of six family members with confirmed Alzheimer’s had low blood levels of B12 while only one of twelve without Alzheimer’s had low levels of B12.7
In still another study demonstrating correlation, researchers collected blood samples from patients before they developed the disease. These samples were compared to samples after they developed the disease. They found that seniors with low intakes of vitamin B12 and folate were twice as likely to develop Alzheimer’s as people with healthy B12 levels.8
In one more study researchers found that Alzheimer’s patients with lower-than-normal B12 levels exhibited more behavioral and psychological symptoms of dementia than patients with normal B12 levels prompting them to conclude “Vitamin B12 could play a role in the pathologenesis of behavioral changes in Alzheimer’s disease.” 9
Multiple Sclerosis and Neurological Disorders
Inadequate levels of vitamin B12 may be misdiagnosed as Multiple Sclerosis or other neurologic diseases in part because the symptoms of B12 deficiency may be identical to neurological disease symptoms. Doctors usually look for blood abnormalities when they check for B12 deficiency however neurological damage can precede blood anomalies by years or even decades. B12 deficiency is common, has many causes and may be found in people of all ages. Yet most doctors believe it to be rare or something that happens in old age. As a consequence whether a patient suffers permanent neurological damage or recovers from inadequate B12 hinges on whether his attending doctor is well informed.
Here are two cases reported in the literature that contrast and dramatize the difference.
Informed Doctor = recovery:
Mystified doctors sent a twenty-eight year old woman to physician Helmut Wilhelm after she developed unexplained vision loss. In addition to checking the woman for other common causes of sudden blindness, Wilhelm found that her serum B12 levels were one-third of the normal limit. he started vitamin B12 injections immediately leading to “an almost complete recovery.” 10
Uninformed and arrogant Doctor = permanent damage:
John Hotchkiss, Jr. MD. practiced in a medical group. One of his partners, a Harvard graduate objected strenuously to his insistence on ruling out B12 deficiency in patients with neurological disorders or other suspicious signs and symptoms. The Harvard doctor grew hostile on more than one occasion when Hotchkiss suggested evaluating a patient’s B12 levels and he refused to be swayed by the medical literature Hotchkiss sent him.
Some years later, Hotchkiss recounted “he sent a patient to me for dizziness evaluation.” Hotchkiss discovered that the woman was not dizzy but instead suffered from poor coordination stemming from neurological dysfunction. He wasn’t surprised because the woman’s history included a gastrectomy 12 years earlier, a surgery that inevitably results in severe B12 deficiency if patients don’t receive compensatory B12 injections.
The woman had been followed by Hotchkiss’ Harvard colleague ever since the surgery, Hotchkiss recounts, “but he had done no follow-up studies concerning her B12 status.” As a result, she suffered from a condition known as “combined systems disease” a complication of chronic B12 deficiency in which damage to the spinal cord tracts causes irreversible crippling.
“The doctor not only failed to monitor her and prevent this from happening, a grave dereliction but he failed to recognize the condition when it occurred”, Hotchkiss recounts. “When we met in the hall some weeks later he said, ‘You got me’.” 11
It has been estimated that up to ten percent of those diagnosed with multiple sclerosis don’t actually have the disease. 12 Most of the time if doctors rule out B12 deficiency in patients suspected of multiple sclerosis they do so by relying on a serum B12 test. This can be inaccurate. Most fail to order other tests such as the urinary MMA test and the plasma Homocysteine test.
Experts (as opposed to doctors in general) believe that a
serum B12 level below 350 pg/ml warrants further testing without regard for the wider reference ranges. The
urinary MMA should be 3.8ug MMA/mg creatine or above. If not then the patient is likely deficient and a plasma homocysteine test will establish if
homocysteine is within the normal range of 4.0 – 12.0 umol/L.13,14
Dr. Eric Norman reported in 2000 that of six women his research team diagnosed with B12 deficiency, three were initially suspected of having multiple sclerosis (MS). These three women’s original doctors were puzzled and diagnosis was delayed because of the similarities between B12 deficiency and MS and because they were young. Dr. Norman commented, “This population deserves further evaluation since it has not been considered prone to cobalamin deficiency.” Proper treatment of his six patients resulted in a nearly total recovery for two and a partial recovery in another. The extent of improvement in two other women could not be measured since treatment had just begun when the report was published and the final woman had not yet developed significant neurologic symptoms. 15
Cases reported in the literature reveal that this is not an isolated case. Another example of B12 deficiency diagnosed as MS was reported in the American Journal of Psychiatry by Dr. Gary Payinda.16
At fifty-two years of age, Mrs. A suddenly developed paralysis in her legs. Her doctor referred her to a neurologist, who diagnosed her with multiple sclerosis. Over the next two months, Mrs. A was placed on numerous medications, but her leg weakness progressed and the drugs did not help. She required a cane, then used a walker and eventually needed a wheelchair to get around. As time went by, Mrs. A became agitated and angry. She grew paranoid and she called the police to report that her family was trying to poison her. She also became violent, throwing furniture and even trying to jump from a moving car.
Mrs. A’s family stunned and frightened by her worsening behavior finally took her to an emergency psychiatric center. She appeared disheveled was delirious and disoriented and paranoid and could not stand without assistance. The psychiatric facility obtained a B12 level which came back extremely low at 9pg/ml.
The doctors diagnosed Mrs. A. with subacute combined spinal cord degeneration and psychosis due to severe vitamin B12 deficiency. Additional tests revealed that she suffered from pernicious anemia; earlier physicians missed the diagnosis in part because her folic acid supplements had masked her blood abnormalities.
Two days after starting B12 injections, Mrs. A. started regaining the strength in her legs. Within eight weeks, her symptoms of mental illness vanished. Unfortunately she may never fully regain her health and mobility because of the delay in diagnosing her correctly. The cause of that delay: her original neurologist failed to diagnose her correctly, instead misdiagnosing her with MS and apparently never considering B12 deficiency.16
Depression
Vitamin B12 deficiency attacks nerves by stripping them of their protective myelin coating and disrupting the communication between brain cells and the nervous system. While this can create the types of symptoms associated with multiple sclerosis it can also affect the nerve cells in the brain that control how one feels, thinks and behaves. Deficiency can cause severe mental illness, including depression, paranoia and even symptoms that resemble schizophrenia.
A few examples will serve to underscore the link between B12 and depression.
Researchers at the National Institute on Aging evaluated a group of disabled women over the age of sixty-five who were active and living independent lives and found that B12 deficiency doubled the risk of severe depression in that group. They concluded that, “It should be an alarming sign that we found a significant rate of B12-deficiency caused depression in this population.”17
In a very comprehensive Netherlands study, researchers screened almost four thousand older individuals for depression and then compared the laboratory test results of those with depressive symptoms to non-depressed control group members. The researchers report that high homocysteine levels, vitamin B12 deficiency and to a lesser extent folate deficiency were all related to depressive disorders. When they controlled for other factors, the effects of homocysteine and folic acid levels were less prominent but low B12 levels were still strongly associated with depression. 18
Here are a few case studies from medical journals:
Doctor G. Daynes reported that in his own practice as medical director of a hospital in South Africa, he successfully treated eight women whose postpartum psychosis stemmed from B12 deficiency. His patients’ recoveries led him to recommend that all women with postpartum psychosis receive large doses of B12. “Where the postpartum psychosis is not primarily caused by lack of vitamin B12, the giving of the preparation will do no harm,” he remarked, “so it seems to me that in all such cases it should be given as soon as possible.”19
Doctors treating a twenty-year old woman, who had attempted suicide three months earlier, discovered the reason for the woman’s urges to kill herself. She had autoimmune pernicious anemia. She now receives regular injections of B12, which have eliminated her depression and suicidal thoughts.20
Dr. Frederick Goggans and colleagues reported a case of an elderly man who suddenly developed severe mania, believing that his hometown was planning a large celebration in his honor, including appearances by Hollywood celebrities. “He became so physically energized,” the doctors wrote, “that six younger men were required to restrain him at the time of admission to the hospital.” Lab tests demonstrated low B12 level and his doctors eventually diagnosed pernicious anemia and treated him with B12 injections. He recovered quickly and at his six-month checkup he as doing well.21
Cardiovascular Problems: B12 – Homocysteine
When vitamin B12 levels drop too low the Methionine Cycle breaks down which results in elevated levels of homocysteine. That cycle converts methionine into smaller molecules one of which is SAMe. SAMe then further breaks down into thousands of compounds and proteins that are vital for healthy cells, tissue and organs. One of those breakdown products is homocysteine. A properly functioning cycle results in homocysteine getting quickly recycled back into methionine with the assistance of vitamin B12 and folic acid. Although there are other pathways for rendering homocysteine harmless, if someone is deficient in B12 the normal functioning of the primary pathway the Methionine Cycle is disrupted. This results in excess homocysteine.
Excess amounts cause blood vessels to lose their elasticity, making it harder for them to dilate and damaging the inner lining. This damage allows cholesterol, collagen and calcium to attach to the inner walls of the blood vessels where they can form sticky deposits called atherosclerotic plaque. These plaques narrow arteries and increase the risk of artery disease, heart attacks, strokes, blood clots and aneurysms.22
Homocysteine is also an oxidant that decreases the production of nitric oxide, a substance crucial to healthy blood vessel function. Decreased levels of nitric oxide are linked to atherosclerosis and high blood pressure.
Homocysteine has been shown to precede the onset of cardiovascular disease.23 Five to ten percent of the population and as many as 30 to 40 percent of senior citizens have high homocysteine levels.24
Link between homocysteine and cardiovascular disease
Researchers in Israel found that male children of heart attack victims had significantly higher homocysteine levels then control group members.25 Furthermore they found that the male children in the top 20 percent were far more likely than others to be in the “parental heart attack” group.
The researchers noted that men in Jerusalem had much higher homocysteine levels then men in the United States which explained the higher heart attack rate. They then added that the difference in homocysteine levels between men in the two countries “was largely attributable to lower plasma vitamin B12 levels in the Israeli population.”25
In a dramatic study reported in the New England Journal of Medicine, Norwegian researchers followed 587 patients with existing coronary artery disease. Within five years of undergoing treatment 11 percent of the patients had died. ‘We found a strong, graded relation between plasma homocysteine levels and overall mortality,” the researchers reported, with about 4 percent of the patients in the low-homocysteine group dying as compared to nearly 25 percent of those in the high-homocysteine group.22 Similar results were found in another study following 400 patients who suffered heart attacks. They discovered that the long-term death rate was more than twice as high in the upper 40 percent of homocysteine levels as it was for other patients.26
More evidence comes from a meta-analysis study which pooled data from seventy-two studies. They concluded that there is “strong evidence that the association between homocysteine and cardiovascular disease is causual”. 27
In young people as well research has demonstrated that high homocysteine is a threat. A large-scale study found that elevated homocysteine nearly doubles the risk of stroke in women between the ages of fifteen and forty-four. The researchers concluded, “The magnitude of the increase in stroke risk was similar to that of smoking a pack of cigarettes per day.”28
B12 lowers homocysteine
Another study, this one short-term (only eight weeks) tested the effects of folic acid alone, B12 alone, and folic acid plus B12 in lowering the homocysteine levels of patients who had suffered ischemic strokes. The researchers found that all three approaches worked but that “the combination therapy yielded the most remarkable result, i.e. plasma total homocysteine was reduced by 38.5 percent.29 A similar short-term study found a 23 percent decrease in homocysteine levels after six weeks of treatment with folic acid and B12.30
Lowering homocysteine reduces cardiovascular problems
Researchers in Switzerland offered homocysteine-lowering therapy to half of a group of 553 patients who had undergone angioplasty to correct coronary artery stenosis (narrowing). After one year, they found that the incidence of “major adverse events” – deaths, nonfatal heart attacks, or the need for repeat angioplasty – was 33 percent lower in the treatment group.31
In another study, the same Swiss research group administered folic acid, B12 and B6 or a placebo to 205 patients who had undergone successful coronary artery angioplasty. They reported that the rate of restenosis (renarrowing of the arteries) was significantly lower in the treatment group than in the placebo group (19.6 percent versus 37.6 percent) and that this group had less than half the need for a repeated procedure. They concluded, “This inexpensive treatment, which has minimal side effects, should be considered as adjunctive therapy for patients undergoing coronary angioplasty.”32
Finally in a study that evaluated eighty-nine men ranging in age from thirty-nine to sixty-seven with existing coronary artery disease, eight weeks of treatment with folic acid and vitamin B12 significantly reduced plasma homocysteine levels compared to controls. Of interest is that they found that the arteries of men taking the vitamins dilated more efficiently in response to blood flow demands. The researchers concluded, “these findings support the view that lowering homocysteine, through B vitamin supplementation may reduce cardiovascular risk.” 33
Even a major pharmaceutical company had at one time no difficulty admitting all of this. A few years ago on Abbott Laboratories Malaysian website they had a section entitled “Homocysteine: The newly proven risk factor for heart attacks”.
On that page were the following sentences:
“Elevated levels of homocysteine might result from lack of certain vitamins which are involved in the breakdown of homocysteine. The vitamins involved are vitamin B6, vitamin B12 & Folic Acid.” 34
“Homocysteine can be easily controlled by providing our body with Folic acid, Vitamin B6 & Vitamin B12 at amounts exceeding the recommended daily allowances.”34
That page is currently only available through the “Internet Archive Wayback machine.”
Inflammation
Let’s reiterate a part of the vitamin B12 uptake process. In the bloodstream, another protein, transcobalamin II (TCII) carries vitamin B12 which started as cobalamin but at the stage of entering the blood stream is in the form of Hydroxocobalamin. The carrier protein, Transcobalamin II (TCII) bound to Hydroxocobalamin enters cells in all tissues via the TCII endocytosis ion channel receptor where after TCII degradation it is converted to Methylcobalamin and 5-deoxyadenosylcobalamin and primarily retained intracellularly. A small portion is however exported via the carriers TCII and Transcobalamin III (TCIII). Methylcobalamin acts in the cytoplasm where it is involved in the Methionine Cycle and 5-deoxyadenosylcobalamin in the mitochondria where it is involved in the Krebs cycle (cellular energy).35
What is of extreme interest is the well-established observation that cobalamin carrier proteins, the Transcobalamins (TCS) are elevated during trauma, infections and chronic inflammatory conditions. This remains to be explained. It has been proposed that such TC elevations signal a need for cobalamin to resolve the inflammatory event.36
Chronic inflammation is usually accompanied by oxidative stress. These factors are primary components of many age-related diseases including cancer, atherosclerosis, neurodegenerative disease and arthritis. Recent studies suggest that cobalamins (vitamin B12 derivatives) may modulate the oxidative stress responses, including those of the inflammatory response. 36
Those studies specifically found:
- Inflammatory diseases are associated with elevated blood levels of transcobalamin (a cobalamin transport protein) 38; and
- It’s (transcobalamin) membrane receptor is up-regulated by TNF-a 39; and
- Cobalamin concentration also modulates TNF-a levels in cerebrospinal fluid. 40
“TNF-a is important in inflammatory responses, so taken together, these observations suggest that elevation of cobalamin could be used to supplement the cellular response to inflammation.”36
There is also an increase in the unsaturated B12 binding capacity.45,46 All of these events seem to occur in chronic inflammation states such as diabetes, Crohn’s disease, rheumatoid arthritis, systemic lupus erythematosus and acute inflammations such as some cancer states, trauma and infections. The increase in transcobalamin carrier proteins and their binding capacity also increase in B12 deficiency. All of this is indicative of a “crying out” for vitamin B12.
In order to appreciate how B12 relates to inflammation let us expand upon the functions we have previously described herein.
In the cell, two enzymes use cobalamin as a cofactor in either the 5-deoxyadenosylcobalamin(AdoCbl) or the methylcobalamin (MeCbl) form.
In the mitochondria AdoCbl is used by the enzyme L-methylmalonyl-CoA mutase in a reaction whereby L-methylmalonyl-CoA is converted to succinyl-CoA, which then enters the Krebs cycle (cellular energy).
In the cytoplasm methylcobalamin (MeCbl) is used by the enzyme methionine synthase in a reaction, (i.e. The Methionine Cycle) whereby tetra-hydrofolate and methionine are generated by a methyl group transfer from methyltetrahydrofolate to homocysteine.41
Homocysteine is a junction metabolite. This means it can be recycled back into the methionine cycle as described above or it can be converted to cysteine via the transsulfuration pathway, ultimately leading to synthesis of the important intracellular antioxidant glutathione. 41
So when the Methionine Cycle is operating optimally the antioxidant glutathione is synthesized and homocysteine does not become elevated as it is fully occupied in either of its two roles.
However elevated homocysteine is associated with endothelial cell (thin layer of cells that line the interior surface of blood vessels) dysfunction. High levels of homocysteine promote the formation of reactive oxygen species (small molecules that are unstable and highly reactive able to create significant cellular damage), primarily by a mechanism involving endothelial nitric oxide synthase (catalyze the production of nitric oxide in blood vessels). 42
Homocysteine also inhibits the antioxidant enzymes superoxide dismutase (important antioxidant defender) and glutathione peroxidase (main biological role is to protect the organism from oxidative damage) and activates endothelial (blood vessel lining) pro-inflammatory signaling pathways. 43
Elevated Homocysteine levels induce cell death in large part because of the inhibition of glutathione. Reduced glutathione levels have been found to correlate with increased oxidative stress, mitochondrial damage, and apoptosis.44 So when it was very recently discovered that cobalamins protect against cell death induced by homocysteine37 part of that beneficial effect was attributed to cobalamin’s ability to increase intracellular clearance of homocysteine through its role in the Methionine Cycle.
However in that study cobalamins were very protective against damage from the reactive oxidative species, Hydrogen peroxide which indicates that they also act as antioxidants via other mechanisms. 37
The recent
Birch study mentioned above was highly significant because it found that cobalamins (specifically thiolatocobalamin) inhibited intracellular peroxide production, maintained intracellular glutathione levels, and prevented apoptotic and necrotic cell death at supraphysiological concentrations. Further these supraphysiological concentrations were not toxic prompting the study to conclude that cobalamins are “powerful but benign antioxidants at pharmacological concentrations.” 37
The study explained their results as follows:
“The antioxidant properties of cobalamin probably result from a combination of direct and indirect effects: stimulation of methionine synthase activity, direct reaction with reactive oxygen and nitrogen species, a glutathione sparing effect, and modification of signaling molecules, leading to induction of stress responses. The remarkably superior protection of thiolatocobalamins in vitro presumably relates to their enhanced function in one or more of these potential mechanisms, the balance of which may differ between the two compounds. In conclusion, cobalamins, and in particular the thiolatocobalamins, exhibit a marked antioxidant activity at pharmacological concentrations and afford significant cellular protection against oxidative stress.”37
Toxicity
Cobalamin is a water-soluble vitamin with a high renal excretion rate and a very safe toxicity profile. Serum levels have been kept as high as 10,000 mcg/ml in infants and children for the long-term treatment of congenital TCII deficiency.47
Hydroxycobalamin has been routinely used in the ICU, in France, and elsewhere, for over 40 years in 4/5 gram iv doses given on up to three consecutive days, as a treatment for cyanide poisoning.48-54 The FDA has granted Hydroxycobalamin orphan drug status for this purpose.54
High dose cobalamin has been used in children, in a 1950s pre-chemotherapy era trial for neuroblastoma where 1000 mcg were given, every other day, for up to 8 years.55
No where in any of these reports is there any indication that high doses led to toxicity. To the contrary, high dose cobalamin is deemed safe.
Cancer
There are certain disease states that result in an elevation in levels of serum cobalamin. Many liver diseases such as hepatitis, cirrhosis and liver cancers as well as leukemias are all accompanied by an increase in circulating cobalamin. This phenomenon is caused predominantly by cobalamin release during what is called “hepatic cytolysis”. Cytolysis is a bursting of the cell and therefore it is not surprising that its contents will be elevated in plasma. Another explanation is that when the liver is in distress there is a decrease in the clearance of compounds, including cobalamin.56
Because of this strong correlation between B12 and cancers you come across studies that find such things as a relationship between vitamin B12 levels and survival in terminally ill cancer patients. In one such study it was found that the length of survival decreased with the increase in serum vitamin B12 levels. The study’s data indicated that an “elevated serum vitamin B12 level is a predictive factor for mortality in patients with cancer.”57
This type of correlation has even led one study58 to draw the erroneous causative conclusion and underscores the need for a determined researcher to discriminate between the conclusions drawn in studies, treating each not as dispositive but rather simply part of an overall picture spanning many multiple disciplines. A researcher that is able to read and draw from a wider array of material is in a better position to come to an understanding.
Vitamin B12 may be elevated in plasma during times of cancer but it is not stimulatory of cancer. The effect of cobalamin on the proliferation of a variety of malignant cells has been examined in vivo and in vitro in numerous studies.59-61 Here are a few very brief examples:
- Methylcobalamin was found to inhibit the proliferation of androgen-sensitive SC-3 cells (a cloned cell line from Shionogi mouse mammary tumor, SC115) in culture at the concentration of 100–300 ug/ml; and
- An inhibitory activity of methylcobalamin on proliferation was also observed in other cell lines (estrogen-sensitive B-1F cells from mouse Leydig cell tumor and MCF-7 cells from human mammary tumor) at the concentration of 500 ug/ml; and
- Large doses of methylcobalamin injected intraperitoneally (100 mg/kg body weight/day) were non-toxic and suppressed the tumor growth of SC115 and B-1F cells in mice fed a vitamin B12 deficient diet.
Vitamin B12 does not in any way stimulate cancer cells. There are no experimental results published indicating that vitamin B12 stimulates growth of malignant cells. In fact these results indicate to the contrary that methylcobalamin
inhibits the proliferation of malignant cells in culture and in vivo. A reading of those studies and others find that often the researchers propose the possibility of methylcobalamin as a potentially useful therapeutic agent for the treatment for some malignant tumors.61
B12 Deficiency and Cancer
One of the strongest scientifically emerging associations is one between breast cancer and B12 deficiency. In a Johns Hopkins study, researchers measured the B12 in blood samples taken from women who had donated blood, comparing samples from 195 women who later developed breast cancer to samples from 195 cancer-free women. Among postmenopausal women, the researchers found those whose B12 levels fell into the lowest fifth were two to four times more likely to develop breast cancer than those in the upper four fifths.67
If you have read this far and hadn’t yet identified a reason to supplement with vitamin B12 for either yourself or people you care about, I believe you have just found one.
In addition to breast cancer, other cancers are being tentatively linked by studies to deficient levels of vitamin B12. Among these are cervical, lung and oral cancers.68-72
One explanation for why deficient B12 levels appear to promote the development of cancer is that the body needs ample B12 in order for folate to work. One of folate’s crucial roles is the synthesis of the nucleotide “building blocks” of DNA. When folate is trapped in unusable form due to a lack of B12 it can not perform this role. This leads to an imbalance in the supply of DNA building blocks, forcing the body to make changes in DNA structure that can make the DNA more vulnerable to breakage. Broken DNA strands can lead to mutations that in turn can lead to cancer. Research demonstrates that chromosome breakage is strongly correlated with deficiencies of either folate or B12 (or with high levels of homocysteine, linked to B vitamin deficiencies) and that large dietary supplements of B12 can minimize this breakage.73
Master Molecule
We have barely scratched the surface and in no way have we even begun to examine the details behind the hypothesis that vitamin B12 is a master molecule which regulates the transcription factor, NFxB thereby determining the extent of the inflammatory response and its subsequent resolution. NFxB is the brain’s master regulator switch in inflammation. Cobalamin (B12) appears to regulate NFxB in both its pro and anti-inflammatory roles. The cascade through which this occurs is simply too complex to be discussed in this paper. To give a quick (but very incomplete) feel for the verity of the hypothesis I will point to a model.
Indirect evidence for Cobalamin/NFxB regulation comes from a model of chronic inflammation. Rheumatoid Arthritis has been treated with some success using high doses of Methycobalamin, one of the active forms of cobalamin, to which Hydroxycobalamin is partially converted intra cellularly.62 An in vitro study to determine cytokine production of monocytes exposed to three mitogens or recombinant Interleukin-2, found Methycobalamin suppressed levels of Interleukin-6 production with three mitogen-stimulation by 66%, 68% and 81%, as compared to controls. Suppression of Interleukin-6 by Methylcobalamin was dose-dependent, and not total.62 Interleukin-6 is believed to be an accurate marker for TNFa activity.63 Both TNFa and Interleukin-6 are pro-inflammatory cytokines (signaling substances) and under run-away inflammatory events such as severe sepsis, and septic or traumatic shock signal the release of still more inflammatory agents. Suppressing their production during periods of inflammation is a sign that Vitamin B12 is regulating NFxB (the inflammation switch).
For a much fuller, detailed look at this hypothesis, three papers by Carmen Wheatley cited below should be read.64-66
Conclusion
You can take steps to lower excess triglycerides, LDL and cholesterol, raise HDL. You can take all the fish oil you want, and modify your diet to lower glucose and reduce insulin. You can modify your lifestyle to avoid hypertension and seek out hormone replacement therapy. But if your levels of homocysteine are excessive all of your changes were for naught. You will suffer from adverse cardiovascular consequences.
Vitamin B12 is a molecule that is vital to maintaining a healthy body. It doesn’t matter whether it proves to be a master molecule. Its presence maintains health and its absence leads to degeneration. It is a molecule that is not toxic if taken in excess. Waiting for the symptoms of malady to appear before introducing vitamin B12 to a regular supplementation protocol may engender deficits that can not be fully overcome. Adding vitamin B12 to a supplementation protocol designed to maintain health and vigor may avoid many of the potentialities discussed herein. Vitamin B12 is by no means a panacea but neither is it snake oil. It is simply a vital molecule of which four out of every ten people are lacking.

 Please Scroll Down to See Forums Below
Please Scroll Down to See Forums Below 












